In the past decade, opioid prescribing in the United States has steadily decreased as federal and state officials implemented strict regulations on prescription opioids to address the opioid crisis. The downward trend sparked concerns of undertreating chronic pain and prompted the Centers for Disease Control and Prevention (CDC) to formally clarify that the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain should not be applied to patients experiencing pain associated with cancer, surgical procedures, or acute sickle cell crises. A new study by CHERISH pilot grant recipient Hao Zhang, CHERISH investigator Yuhua Bao, and colleagues provides evidence for those concerns and found that patients with cancer-related pains faced a decline in opioid dispensing from 2011 to 2017.
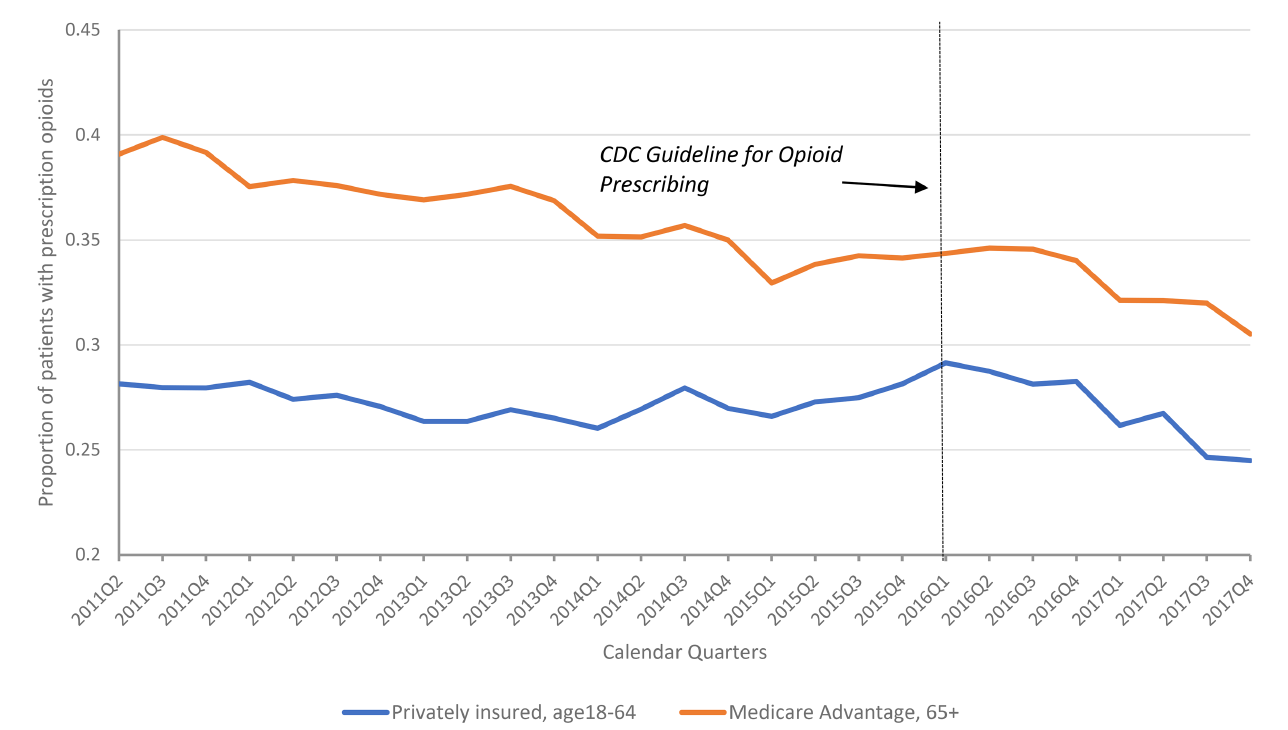
Percentage of patients experiencing cancer with bone metastasis who had at least one day of prescription opioids in a calendar quarter: Q2 of 2011 to Q4 of 2017.
Published in The Oncologist, the research found that the rate of opioid dispensing and the amount of opioids dispensed for patients experiencing cancer with bone metastasis decreased. Sourcing data from the Health Care Cost Institute, a nationally representative database of commercial insurance claims, Zhang and colleagues identified privately insured patients aged 18 to 64 and Medicaid Advantage enrollees aged 65 or older. They found that for both populations, the percentage of patients with at least one day of prescription opioids during a quarter declined; the total morphine milligram equivalents in both populations also declined. Among both privately insured patients and Medicaid Advantage enrollees, the average daily morphine milligram equivalents and the average number of days covered by opioids in a quarter also declined.
Patients experiencing cancer with bone metastasis are often prescribed opioids and additional therapies to manage chronic pain. While the 2016 CDC guidelines were not intended to affect patients with chronic pain, sickle-cell disease, or surgical procedures, findings from Zhang and colleagues’ study raise the concern that these patients have reduced access to prescription opioids for pain management. The authors encourage future research to examine if opioid prescribing guidelines may unintentionally lead to higher rates of undertreated pain for cancer patients.
This research was funded by a CHERISH pilot grant awarded to Dr. Hao Zhang in 2020 and a grant from Arnold Ventures.
Additional contributions are acknowledged from CHERISH Research Affiliate Katherine Wen and Weill Cornell Medicine colleague Phyllis Johnson for their support in HCCI data management.
This article originally appeared in the CHERISH blog.
- Highlights

